Prevent Overtraining Syndrome and Overuse Injuries in Youth Sports
Helping parents, coaches, and young athletes understand overtraining syndrome (OTS), the specific injuries associated with overuse, early signs of detection, and general guidelines for training.
Overtraining in Youth Sports
With over 30 million youth sports participants ages 6 to 18, it is important for parents and coaches to know about overtraining syndrome (OTS), the specific injuries associated with overuse, early signs of detection, and general guidelines for training.
Every year more children and adolescents are participating in organized and recreational sports. This is a great sign in the fight against childhood obesity as it builds lifelong physical activity habits, promotes healthy competition, and builds skills for future opportunities. Unfortunately one of the downsides with increased activity in youth sports is the increased risk of overtraining, overuse injuries, and burnout.
What is Overtraining Syndrome (OTS)?
Overtraining Syndrome (OTS) is more commonly referred to as “burnout”. OTS or “burnout” is caused by intensely working the body for long amounts of time without allowing the time for rest and recovery.
The American Academy of Pediatrics describes overtraining syndromes as a “series of psychological, physiologic, and hormonal changes that result in a decreased athletic performance. With so many options such as football, gymnastics, swimming, wrestling, and tennis at all levels; kids have naturally become more likely to suffer from injury.
What is an Overuse Injury?
Overtraining can directly cause an overuse injury. Overuse injuries often include damage to bone, muscle, and tendons. These injuries can be classified into 4 stages:
- Pain in the affected area after physical activity
- Pain during physical activity, but not restricting performance
- Pain during physical activity that also restricts performance
- Chronic, persistent pain, even at rest
Because young athletes’ bodies are still developing, they are more susceptible to overuse injuries. Their bones are still growing, therefore cannot handle as much stress as fully developed adults. Generally, the best way to prevent major overuse injuries is to understand and identify the young athlete who is at most at risk.
If your young athlete is showing signs of injury, it is always a good idea to get a professional assessment. A physical therapist can diagnose the injury and provide a treatment plan to safely return to competition. Contact Balanced Physical Therapy to schedule a free injury screening or comprehensive evaluations here.
Common Overuse Injuries in Youth Sports
Some examples of overuse injuries and risks that may result from overtraining in youth sports include:
Little league and travel baseball players can be at risk for throwing injuries such as medial apophysitis or “little leaguer’s elbow”. Too much overhand throwing, especially with poor technique, can result in excess inflammation and irritation in the elbow. This can have long-lasting effects on the medial apophysis growth plate.
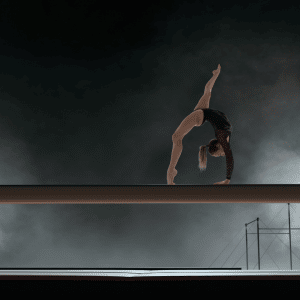
A child or adolescent gymnast can be at risk for developing spondylosis (pain in the spine due to deterioration) when doing repetitive hyperextension and rotation while participating.
Young swimmers are susceptible to shoulder injuries such a rotator cuff or bicep tendonitis, shoulder impingement, and neck pains.
Track and distance runners often develop shin splints and stress fractures as a result of overtraining.
These injuries are commonly caused over time, and not suddenly. This is good news, especially for parents and coaches who know the signs of overtraining and overuse.
Signs of Overtraining and Burnout
Parents and coaches concerned about the possibility of overtraining have multiple ways to tell when a young athlete needs more time to rest and recover. The Boston Children’s Hospital lists common signs of overtraining that include:
- Slower times in distance sports
- A decrease in athletic performance
- Decreased ability to achieve training goals
- Decreased motivation to practice
- Young athlete getting tired easily
- Irritability and unwillingness to work with teammates
- Disturbance in sleep schedule
- Weight loss or appetite changes
How To Prevent Overtraining Syndrome
General guidelines suggest that to promote fun, develop skills, and achieve individual goals; a young athlete requires good training and rest balance. Some ways to prevent overuse injuries and burnout include:
- Encourage young athletes to take 1-2 rest days per week. This allows time to recover physically and psychologically between competition.
- Advise young athletes that their weekly training time, repetitions, or total distance should not increase more than 10% per week.
- Encourage athletes to take a seasonal rest from a single sport for 2-3 months a year. Taking breaks and developing other skills are essential for preventing injuries.
- Focus on proper nutrition, hydration, and sleep.
- Be mindful and cautious when entering multiple tournaments on consecutive weeks
- Be consistent with yearly checkups with pediatricians and family physicians.
- Emphasize that the reason we participate in sports is to have fun, develop healthy lifestyle habits, and improve athletic skills.
Using these guidelines, parents, coaches, and healthcare professionals can help keep young athletes injury-free. Mixing in rest days and diversifying the activities kids participate in can help tremendously when developing skills and avoiding burnout.
Prevent Overtraining Syndrome and Overuse Injuries in Youth Sports Read More »










