Barbell Rehab Method: Injury Rehab & Managing Chronic Conditions
Barbell Rehab Method (BRM)
The Barbell Rehab Method is an approach to physical therapy that integrates principles from strength training and rehabilitation to help individuals recover from injuries or manage chronic conditions. It emphasizes using barbell exercises to improve strength, mobility, and function while addressing specific movement dysfunctions or imbalances.
Barbell Rehab Method In Action
The Barbell Rehab Method is typically used in physical therapy during:- Assessment: The therapist assesses the individual’s movement patterns, strength deficits, range of motion, and any specific impairments related to their injury or condition. This assessment helps tailor the rehabilitation program to the individual’s needs.
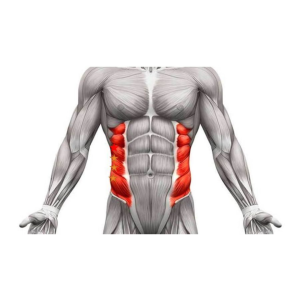
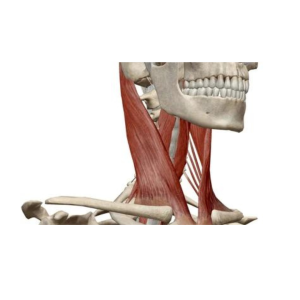
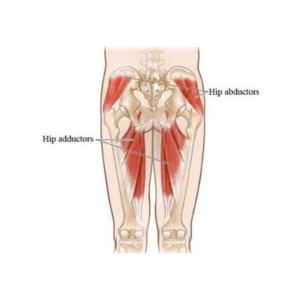
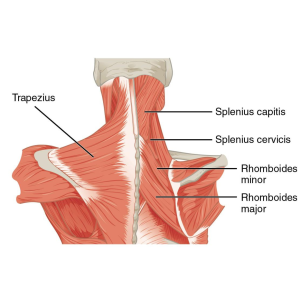
- Exercise Prescription: Based on the assessment findings, the therapist prescribes specific barbell exercises designed to target areas of weakness or dysfunction. These exercises may include squats, deadlifts, presses, rows, and other compound movements that engage multiple muscle groups.
- Technique Instruction: Proper technique is crucial to prevent further injury and maximize the effectiveness of the exercises. The therapist provides detailed instructions on performing each exercise safely and effectively, paying close attention to posture, alignment, and movement mechanics.
- Progression: As the individual progresses in their rehabilitation, the therapist gradually increases the intensity, load, or complexity of the exercises to continue challenging their strength and mobility. This progressive approach helps promote ongoing improvement and prevents plateaus in recovery.
- Individualization: The Barbell Rehab Method is highly individualized, considering each person’s unique goals, abilities, and limitations. The therapist may modify exercises or incorporate additional strategies, such as mobility drills or accessory movements, to address specific needs and optimize outcomes.
- Education and Empowerment: Throughout the rehabilitation process, the therapist educates the individual on proper body mechanics, injury prevention strategies, and self-management techniques to support long-term health and wellness. The Barbell Rehab Method promotes independence and self-efficacy by empowering individuals to actively participate in their recovery.
Barbell Rehab Method For All Ages & Activity Levels
The Barbell Rehab Method can be applied to individuals of different age groups and activity levels by tailoring the rehabilitation program to meet each individual’s specific needs, goals, and capabilities. Here’s how it can be adapted for different populations:Young Adults and Athletes:
-
- Young adults and relatively active athletes with a higher fitness level may focus on restoring strength, mobility, and function to facilitate a safe return to sports or other high-intensity activities.
- The rehabilitation program may include more advanced barbell exercises and progressions, such as plyometric variations, dynamic movements, and sport-specific drills, to challenge their strength and athleticism.
- Through targeted strength and conditioning protocols, emphasis is placed on optimizing movement mechanics, enhancing performance, and reducing the risk of future injuries

Middle-Aged Adults:
-
-
- Middle-aged adults may benefit from the Barbell Rehab Method to address age-related changes, musculoskeletal issues, or injuries related to work, daily activities, or recreational pursuits.
- The rehabilitation program focuses on improving functional capacity, reducing pain, and enhancing overall quality of life by targeting weakness, stiffness, or dysfunction areas.
- Exercises are selected and modified based on individual capabilities and goals, emphasizing improving movement patterns, joint mobility, and muscular strength to support daily activities and maintain independence.
-

Older Adults:
-
- The Barbell Rehab Method can help older adults address age-related strength, balance, and mobility declines and manage chronic conditions such as osteoarthritis or osteoporosis.
- The rehabilitation program emphasizes safe and effective exercises that improve muscular strength, bone density, joint stability, and functional capacity to support healthy aging and prevent falls or injuries.
- Exercises are selected and progressed cautiously, considering factors such as joint health, balance impairments, and mobility limitations. Modifications may include using lighter weights, incorporating balance training, and focusing on functional movements relevant to daily activities.

Sedentary or Deconditioned Individuals:
-
- Sedentary or deconditioned individuals may benefit from the Barbell Rehab Method to improve overall fitness, health, and well-being and manage chronic conditions such as obesity, diabetes, or cardiovascular disease.
- The rehabilitation program focuses on gradually reintroducing physical activity, building foundational strength, and improving movement mechanics to support long-term adherence and sustainable lifestyle changes.
- Exercises are selected and progressed based on individual fitness levels and tolerance, emphasizing gradual progression, proper technique, and personalized support to overcome barriers and build confidence in physical activity participation.
 The Barbell Rehab Method can be adapted to individuals of different age groups and activity levels by customizing the rehabilitation program to address their unique needs, capabilities, and goals. Whether recovering from an injury, managing a chronic condition, or striving to improve overall health and fitness, strength training and rehabilitation principles can be effectively applied to promote optimal outcomes and enhance quality of life across the lifespan.
The Barbell Rehab Method can be adapted to individuals of different age groups and activity levels by customizing the rehabilitation program to address their unique needs, capabilities, and goals. Whether recovering from an injury, managing a chronic condition, or striving to improve overall health and fitness, strength training and rehabilitation principles can be effectively applied to promote optimal outcomes and enhance quality of life across the lifespan. Become A Patient
Schedule an Appointment
Barbell Rehab Method: Injury Rehab & Managing Chronic Conditions Read More »