Muscle Imbalances: A Comprehensive Guide From A Physical Therapist
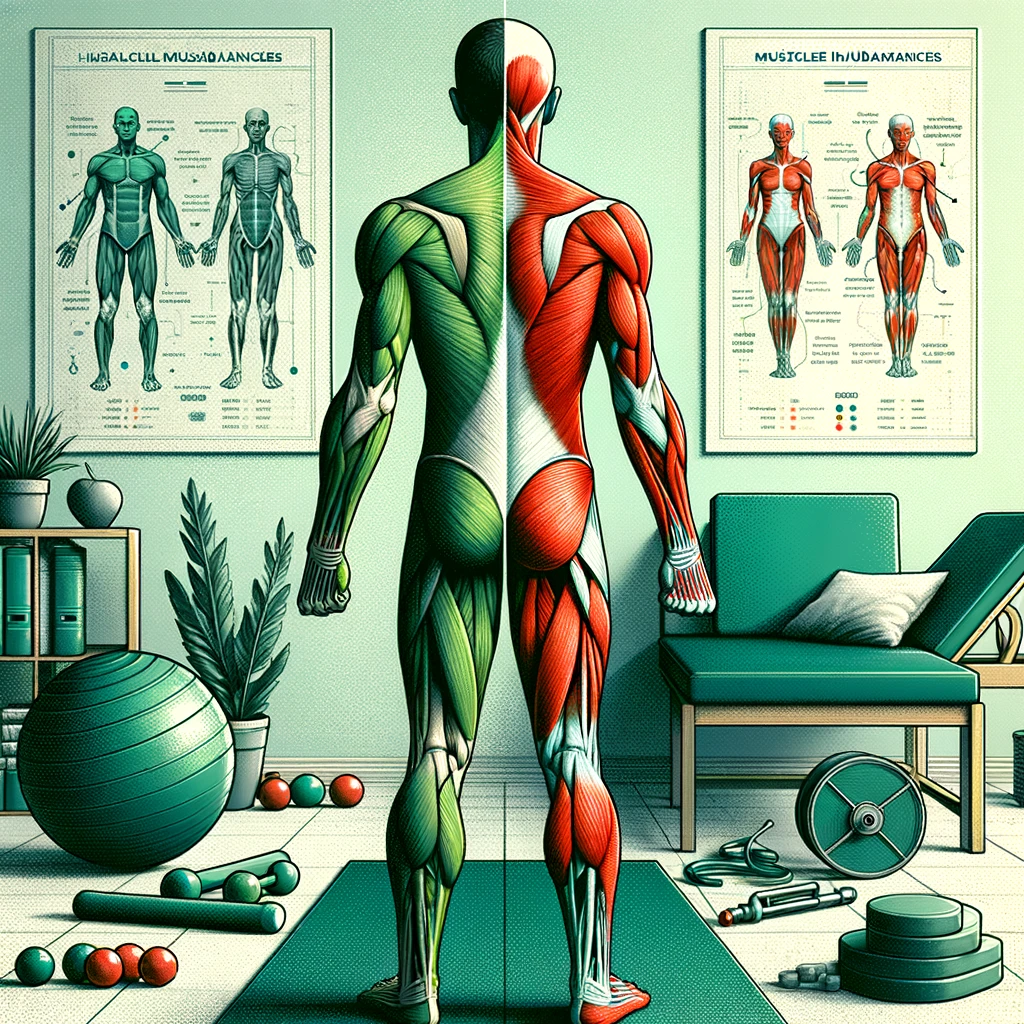
Understanding and Addressing Muscle Imbalances
Muscle imbalances occur when there’s a significant difference in the strength or size of muscles on opposite sides of the body or within different parts of the same muscle group. These imbalances can compromise our body’s ability to perform efficiently and effectively, leading to a heightened risk of injuries and a potential decrease in overall physical performance. Recognizing and addressing these imbalances is crucial for anyone looking to maintain optimal body function, whether you’re an athlete, a weekend warrior, or someone navigating the challenges of everyday activities. This comprehensive guide explores the causes, symptoms, impacts, and corrective strategies for muscle imbalances, emphasizing the pivotal role of physical therapy in managing this widespread issue.What Causes Muscle Imbalances?
Muscle imbalances can arise from various factors, often interlinked, ranging from everyday habits to more complex health conditions. One of the primary culprits is poor posture, especially given the increasing prevalence of sedentary lifestyles that promote sitting for prolonged periods. This lifestyle can lead to the weakening of postural muscles and the overuse of their opposites, setting the stage for imbalance. Incorrect exercise techniques or an unbalanced focus on certain muscle groups can further exacerbate these imbalances. For example, consistently favoring chest exercises while neglecting the upper back can lead to a forward-hunched posture, a common imbalance scenario. Additionally, inherent physiological conditions, such as scoliosis (a curvature of the spine) or discrepancies in limb lengths, can predispose individuals to developing muscle imbalances from an early age.Recognizing the Signs of Muscle Imbalances
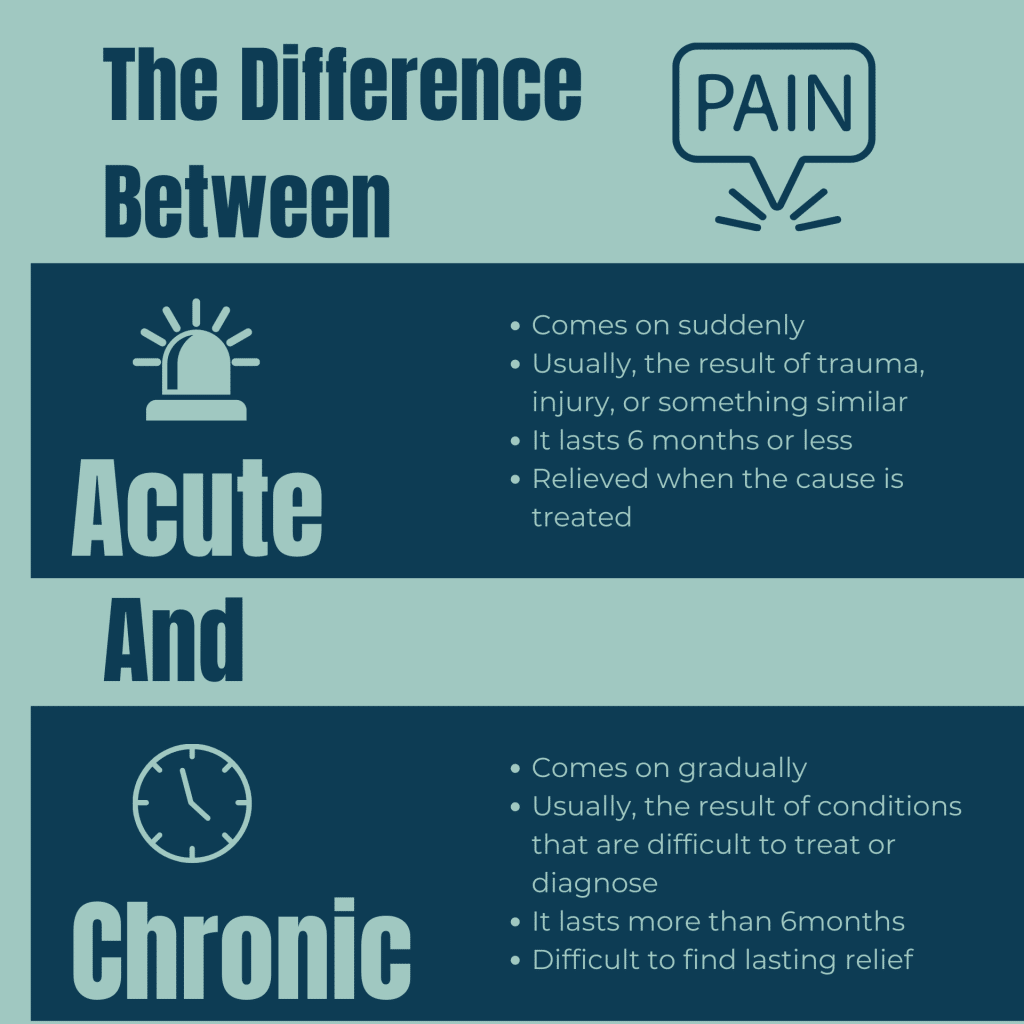
Spotting muscle imbalances involves paying attention to several key indicators. Uneven muscle size or strength between the left and right sides of the body can be a clear sign, as can persistent joint pain or discomfort that doesn’t stem from acute injury. A limited range of motion and a noticeable decrease in strength or stability on one side can signal an underlying imbalance. These symptoms are physical markers and can lead to compensatory patterns, where the body adjusts in potentially detrimental ways to maintain function. Given these complexities, professional diagnosis becomes crucial. A physical therapist can assess your condition through a detailed examination, identifying specific imbalances and crafting a tailored plan for correction.Top 5 Muscle Imbalances Treated by Physical Therapists
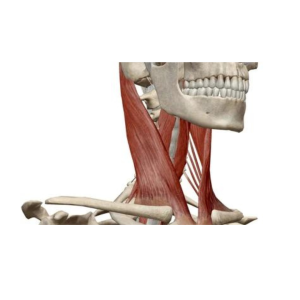
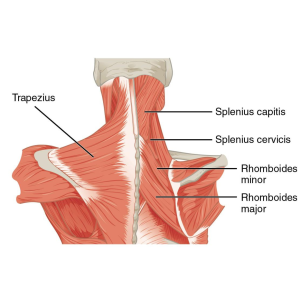
Physical therapists encounter a wide range of muscle imbalances in their practice. Here are five of the most common imbalances we treat, which underscore the diverse impact these issues can have on the body:- Upper Crossed Syndrome (UCS) is characterized by tightness in the upper back and neck muscles and weakness in the front of the chest and shoulders. It is commonly seen in individuals who spend long hours sitting, leading to a forward head posture and rounded shoulders.
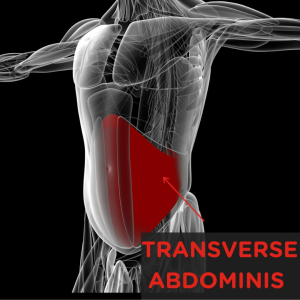
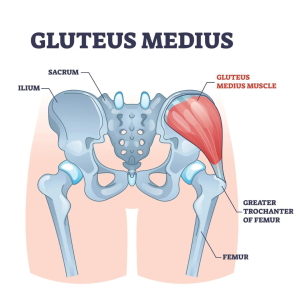
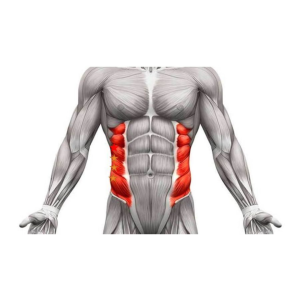
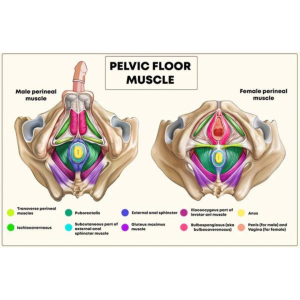
- Lower Crossed Syndrome (LCS): This imbalance involves tightness of the lower back and hip flexor muscles and weakness in the abdominal and gluteal muscles. LCS often manifests as an exaggerated lumbar curve, contributing to lower back pain.
- Anterior Pelvic Tilt: This condition stems from tight hip flexors, lumbar erector muscles, and weakened abdominal and gluteal muscles. It leads to a forward tilt of the pelvis, potentially causing lower back discomfort and altered posture.
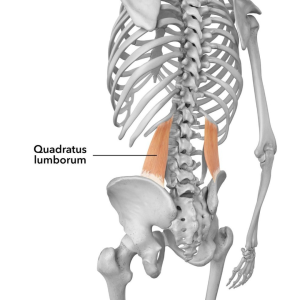
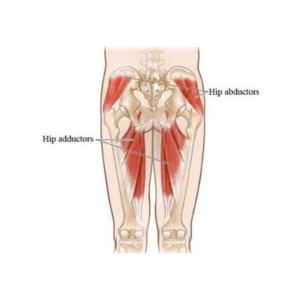
- Lateral Pelvic Tilt: Caused by an imbalance in the muscles that control the pelvis’s side-to-side movement, resulting in one hip being higher than the other. This imbalance can contribute to uneven stress distribution across the lower back, hips, and knees.
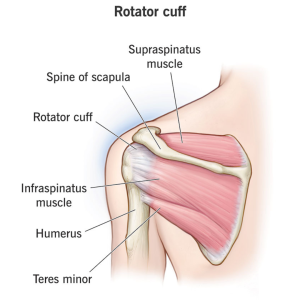
- Shoulder Impingement Syndrome: This condition often results from imbalances in the shoulder muscles. Tightness in the chest and weakness in the upper back and rotator cuff muscles narrow the space for shoulder movement, which can cause pain and restrict the shoulder’s range of motion.
The Impact of Muscle Imbalances on Daily Life
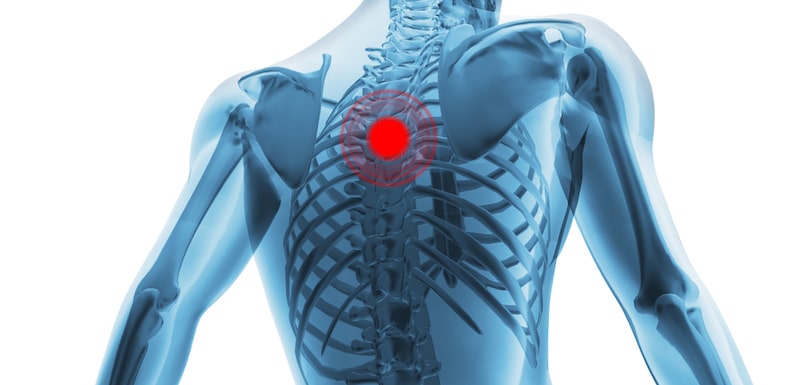
The consequences of untreated muscle imbalances extend far beyond the gym. They can alter how you walk, run, or engage in any physical activity, increasing the risk of injuries by forcing the body into unnatural compensation patterns. Over time, these imbalances can lead to chronic pain, reduced mobility, and a diminished quality of life, affecting everything from your ability to perform daily tasks to your overall well-being.
Strategies for Correcting Muscle Imbalances
Addressing muscle imbalances requires a multi-faceted approach, ideally under the guidance of a physical therapy professional. Treatment strategies often include a combination of strengthening exercises for underused muscles, stretching and flexibility routines for overused or tight muscles, and modifications to everyday activities to prevent further imbalance. Physical therapy is critical in this process, offering personalized assessments and recommendations based on your unique needs and goals. Techniques such as targeted exercises, manual therapy, and education on proper posture and movement patterns can all contribute to restoring balance and function.Preventing Muscle Imbalances
Prevention is equally as important as correction. Maintaining a balanced exercise regimen that includes strength training and flexibility work can help prevent muscle imbalances. Regular physical activity, proper exercise techniques, and good daily posture are fundamental to prevention. Additionally, periodic check-ups with a physical therapist can help catch and address any emerging imbalances before they develop into more significant issues.Conclusion
Muscle imbalances, while common, can significantly impact your quality of life and physical performance if left unchecked. You can ensure that these imbalances don’t hold you back through early recognition, understanding the root causes, and taking proactive steps toward correction and prevention. Remember, seeking the expertise of physical therapy professionals is crucial in navigating the path to a balanced, healthy body. Whether you’re looking to enhance your athletic performance or move through life with greater ease, addressing muscle imbalances is a step in the right direction toward achieving your health and fitness goals.Become A Patient
Schedule an Appointment
Muscle Imbalances: A Comprehensive Guide From A Physical Therapist Read More »